We’ve answered many different kinds of questions for many different organisations in over 70 countries. They include:
Poor diet contributes to the high prevalence of hypertension, obesity and non-communicable diseases (NCDs), such as cardiovascular diseases, cancers and diabetes, in Europe. In particular, high levels of salt consumption are harmful to the cardiovascular system. Therefore, a comprehensive strategy to improve diet, including reducing the levels of salt consumption is widely recognised as a strategy to improve health at a population level.
For this study, the British Heart Foundation commissioned HealthLumen to develop a microsimulation model to quantify the significant health and economic benefits that could be achieved by 2035 if UK adult salt consumption was reduced to 6g per day, as per current recommendations, by 2024 and 5g per day by 2030, in line with the WHO target.
Results show that a reduction in salt consumption could attenuate the health and economic burden of hypertension, CHD and stroke. Under the intervention (salt reduction) scenario, we project that 1.4 million fewer people will be living with hypertension in 2035 compared to the baseline scenario. We project that 134,789 cumulative incidences of CHD and 48,540 cumulative incidences of stroke could be avoided by 2035. We project that these reductions will incur direct cost savings of £6.70 billion and indirect cost savings of £4.70 billion between 2021 and 2035.
Given the health and economic benefits that would be generated by a reduction in daily salt consumption, UK Government action that seeks to enforce the national salt reduction policy outlined in this report would contribute significantly to the 2019 NHS target of preventing “up to 150,000 heart attacks, strokes and dementia cases over the next 10 years.”
View blog post
Obesity prevalence is increasing across Europe, which is contributing to an increase in the incidence of liver and cardiovascular disease, already adversely affected by relatively high levels of alcohol consumption. This study demonstrates the effect of rising obesity prevalence on liver diseases, assuming no change in current alcohol consumption, and the associated economic burden to the French, Dutch and Romanian healthcare systems, as well as the potential benefits of reduced BMI and alcohol consumption in these countries. The data suggest that policies designed to impact on both risk factors may be of benefit to population health, and that even small changes in these risk factors can lead to significant outcomes.
Accurately projecting the incidence of NCDs requires the joint prevalence distributions of several relevant risk factors. For example, body mass index (BMI) and air pollution are risk factors for type 2 diabetes; alcohol consumption and BMI are risk factors for Chronic Liver Disease; smoking and air pollution are risk factors for lung cancer. However, in most cases, relative risks for diseases have been calculated for individual risk factors only, with joint relative risks for multiple risk factors available only in a small number of cases.
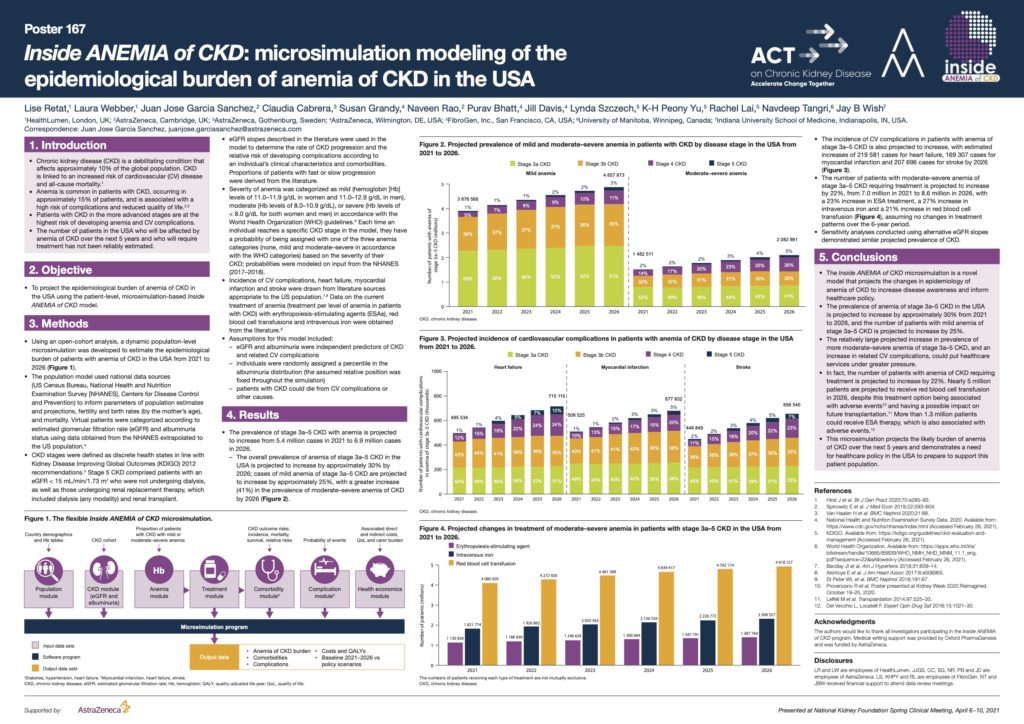
Chronic kidney disease (CKD) is a debilitating condition that affects approximately 10% of the global population. Anemia is common in patients with CKD, occurring in approximately 15% of patients, and is associated with a high risk of complications and reduced quality of life.
The number of patients in the USA and Canada who will be affected by anemia of CKD over the next 5 years and who will require treatment has not been reliably estimated. This study, commissioned by AstraZeneca, projects the epidemiological burden of anemia of CKD in the USA and Canada using a patient-level, microsimulation-model.
In the USA the prevalence of stage 3a–5 CKD with anemia is projected to increase from 5.4 million cases in 2021 to 6.9 million cases in 2026. In Canada, the prevalence of anemia of stage 3a–5 CKD is projected to increase from approximately 1.5 million patients in 2021 to 2.2 million patients in 2026.
The projected increasing prevalence of advanced CKD and associated anemia, as well as the estimated increases in numbers of related cardiovascular (CV) events and patients who will require treatment, could put healthcare systems under greater pressure, and demonstrates a need for healthcare policy in the USA and Canada to prepare to support this patient population.

Air pollution has an adverse effect on people’s health, both in the long- and short-term. The Guy’s and St Thomas’ Charity commissioned HealthLumen to undertake a project to quantify the impact of air pollution on the health of the populations of the London boroughs of Lambeth and Southwark. In these areas, the majority of air pollution comes from road traffic, but also from heating and construction emissions. A number of policies have been put in place London-wide to reduce air pollution emissions and therefore prevent related impacts (for example ULEZ and BreatheLondon), as well as locally in Lambeth and Southwark. The findings of this study build on the existing body of knowledge on this topic by quantifying the impact of specific scenarios on air-pollution related health burden.
The key conclusions are that borough-specific and pan-London actions are required alongside local and national legislation and policy if larger health benefits and cost savings are to be made. It is clear that measures to maintain levels of NO2 emissions found during the COVID-19 lockdown and to meet the WHO levels for PM2.5 would have significant health and cost benefits for both Lambeth and Southwark.
View blog post
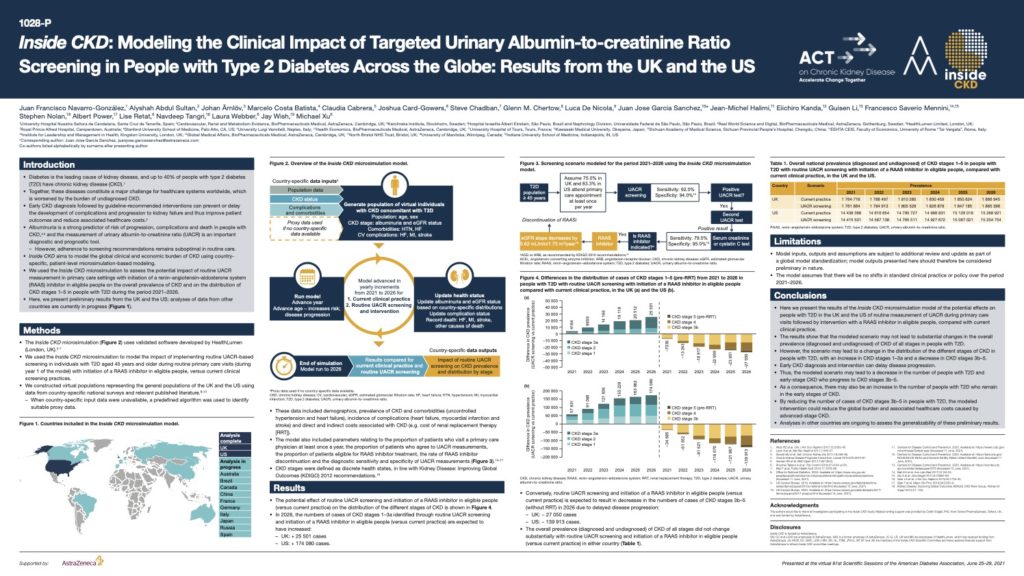
Diabetes is the leading cause of kidney disease, and up to 40% of people with type 2 diabetes (T2D) have chronic kidney disease (CKD) Together, these diseases constitute a major challenge for healthcare systems worldwide, which is worsened by the burden of undiagnosed CKD. Early CKD diagnosis followed by guideline-recommended interventions can prevent or delay the development of complications and progression to kidney failure and thus improve patient outcomes and reduce associated healthcare costs.
Albuminuria is a strong predictor of risk of progression, complications and death in people with CKD and the measurement of urinary albumin-to-creatinine ratio (UACR) is an important diagnostic and prognostic tool.
This poster, presented at the virtual American Diabetes Association’s 81st Scientific Sessions, June 25–29, 2021 demonstrates the potential effects on people with T2D in the UK and the US of routine measurement of UACR during primary care visits followed by intervention with a RAAS inhibitor in eligible people, compared with current clinical practice. By reducing the number of cases of CKD stages 3b–5 in people with T2D, the modelled intervention could reduce the global burden and associated healthcare costs caused by advanced-stage CKD.
We have an experienced and multi-disciplinary team of software engineers, population health and policy research experts, and mathematicians.
Team